Urticaria, commonly known as hives, along with allergic rhinitis¸ allergic asthma, all can be considered diseases of affluence; that is because they happen much often in societies with increasing wealth and developments. Urticaria patients have rashes, hives or wheals on their skin that is painfully itchy. Accordingly to clinical statistics, “At any given time, the prevalence of chronic uritcaria is up to 1% of the world’s population.” When the painful hives spontaneously present and reoccur for more than six week, it is considered as Chronic Spontaneous Urticaria (CSU), and two thirds of Chronic Uriticaria have CSU.
CSU is not an allergic disease. Its cause remains unknown. A large percentage of patients have autoimmune problems. According to clinical trial cases, there are patients whose skin cannot be exposed to temperature lower than fifteen celcius degrees such as to tap water. Usually doctors prescribe anti-histamines for such patients to relieve the itchy symptoms, however, roughly twenty percent of such cases remain living miserably. The good news is, lately, the EU countries, U.S.A., and about 10 other countries have approved the use of Xolair for CSU patients who are not responding to H1-antihistamines treatment.
 Dr.Marcus Maurer (left) and Tse Wen Chang (right)Dr. Tse Wen Chang, who is a distinguished research fellow at Genomics Research Center, is the creator of the anti-IgE drug (omalizumab, trade name Xolair). The primary function of Xolair lies in its binding to IgE. IgE is an antibody inside human body that has been identified as a major mediator of several allergic symptoms. The fields of dermatology and clinical immunology are puzzled how Xolair can treat CSU. Dr. Chang has teamed up with Dr.Marcus Maurer and published a review on The Journal of Allergy and Clinical Immunology to elucidate the molecular mechanisms behind the success of the trials. Dr. Marcus Maurer is the Director of Research at the Department of Dermatology of Charité – Universitätsmedizin in Berlin, Germany, as well as the lead physician of the international phase II and III clinical trials of Xolair in CSU.
Dr.Marcus Maurer (left) and Tse Wen Chang (right)Dr. Tse Wen Chang, who is a distinguished research fellow at Genomics Research Center, is the creator of the anti-IgE drug (omalizumab, trade name Xolair). The primary function of Xolair lies in its binding to IgE. IgE is an antibody inside human body that has been identified as a major mediator of several allergic symptoms. The fields of dermatology and clinical immunology are puzzled how Xolair can treat CSU. Dr. Chang has teamed up with Dr.Marcus Maurer and published a review on The Journal of Allergy and Clinical Immunology to elucidate the molecular mechanisms behind the success of the trials. Dr. Marcus Maurer is the Director of Research at the Department of Dermatology of Charité – Universitätsmedizin in Berlin, Germany, as well as the lead physician of the international phase II and III clinical trials of Xolair in CSU.
The majority of Chang’s research has been studying the actions and impacts of IgE, and how to stop IgEs from causing more negative impacts. In the early days, he had gone through entrepreneurship phases and performed successful clinical trials for allergic rhinitis pinpointing IgE; later, big pharmaceutical companies carried out extensive clinical trials on various allergic diseases, and successfully marketed the drug under the name Xolair to treat allergic asthma. Xolair has been approved in many countries, including Taiwan, and allergic asthma patients without help previously are in safe hands now.
About six years ago, some dermatology physicians in the U.S.A. tested out Xolair to help the CSU patients who are suffering long term torturing of the itch and pain, as one after another positive case reports popped up, extensive clinical trials executed throughout multiple countries were organized.
Although Xolair has proved clinically effective to treat CSU, it is still left to the scientist to explain the mechanisms. Generally speaking, CSU is considered an auto-immune disorder symptom, as opposed to allergic reactions. In the published report, Chang explained the potential pharmacologic mechanisms.
As described by Dr. Chang, most allergies are due to the existence of IgE. In the primitive environments, there are many parasites, when human beings were infected, IgE was designed to recognize and grab such intruders. IgE would grab the intruders, and sit on the receptor molecule on mast cells.
Mast cell is a very import character in the whole scenario of inflammation. A mast cell exists in the skin layer, and its various receptors are acting as alarms. When the IgE specific alarm FcεRI receptors on mast cell catch enough IgEs grabbing intruders on hand, they create a crosslink effect, and then, the mast cell knows it’s time to make ammunitions and start the combat by releasing the ammos. As a result, histamine and other inflammatory mediators are released. Such process is called degranulation. Basophils is similar to mast cell except that it floats inside circulation system.
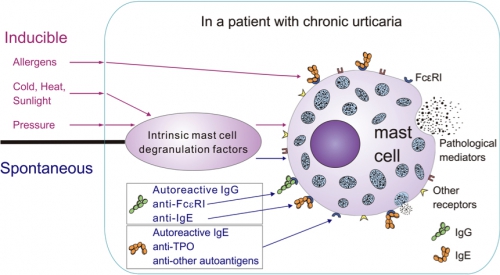 |
| Figure 1. The inflammatory manifestation of mast cells in affected skin is the final common pathway for various types of urticaria. |
Although CSU generally is considered a disease in the auto immune category, as opposed to allergies which are triggered by specific antigens, the reason why Xolair can treat auto immune diseases were explained. There are several identified causes for CSU, including a substance produced by human thyroid called Thyroperoxidase (TPO) that are mistaken by IgE as antigens; there is also another antibody IgG produced by human body, yet IgG can interact with IgE or through the FcεRI receptor to mast cell directly; all these are false alarms, yet can trigger mast cell or basophil to start the combat mission.
Furthermore, while there are much less IgE around, mast cell seem to be even more on alert for its designated duties, and researchers observed a situation when the crosslinks were not quite taken places, and the mast cell were so alerted already that it started the whole degranulation processes when a few IgE show up. That explains why the hives can appear so quickly out of no significant outside stimulations.
Nowadays, in the much developed societies, people are not infected by parasitic worms, and the need to detect and combat is lowered. It has been observed that the receptors for IgE is relatively lowered in number. If there is no need for it, perhaps the whole mechanism should be eliminated?
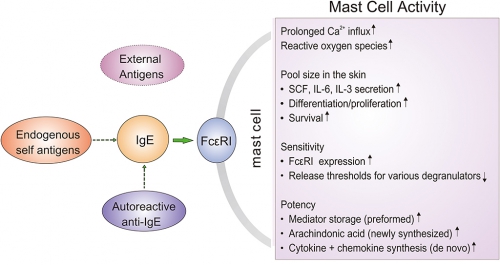
Indeed, by studying in the molecular scale, the group has spotted a situation when IgE being neutralized, the receptors on mast cell tend to be recycled by itself and thus less. The mast cell with less receptors appears to be laid back, make less ammos, and thus create less infectious symptoms.
 |
|
Figure 2. The binding of IgE to the high-affinity receptors (FceRI) on mast cells can elevate |
The conclusion can be “no IgE, no infection”. Therefore, treating with Xolair to eliminate IgE can ultimately eliminate the whole unnecessary inflammatory mediator releasing process because it not only traps IgE surrounding mast cells, it also trap IgEs floating around on basophils.
Dr. Chang has accumulated so much insights regarding IgE, and his invention has already helped lots of patients globally. Nonetheless, he expressed concerns toward other diseases with similar analogies, and he also feels confident to be able to help those others in days to come.
The review about Xolair and CSU titled ‘The Potential pharmacologic mechanisms of omalizumab in patients with chronic spontaneous urticarial’ has been published on June 17, 2014 on-line in The Journal of Allergy and Clinical Immunology.