As normal cells undergo abnormal proliferation, morphological changes, and eventually transform into cancer, there is a transitional phase known as "precancerous lesions" in pathology. Pancreatic Intraepithelial Neoplasia (PanIN) is the most common and earliest form of precancerous lesion in pancreatic cancer. Current literature indicates that over 90% of PanINs and pancreatic cancer cases exhibit mutations in the KRAS gene. However, can the mutation of the KRAS gene alone drive the early formation of PanINs? Certainly, "there is more than one truth."
Under the leadership of Dr. Wen-Hwa Lee and Dr. Chun-Mei Hu, the research team at the Genomic Research Center dedicated five years to employing advanced whole pancreas 3D histological techniques for the dissection of KrasG12D/+ genetically modified mice. Their investigation confirmed that more than 90% of early-stage PanIN cells exhibit overexpression of the Muc4 gene, a mucin, and are surrounded by activated fibroblasts. Moreover, they unveiled the reciprocal interaction between the cancer-causing Kras gene and the mediated Muc4 gene. This dynamic interplay modifies and attracts neighboring fibroblasts, assimilating them as allies in promoting pancreatic carcinogenesis. Through a synergistic effect, a microenvironment favoring PanIN cell proliferation is established, elevating the susceptibility to precancerous lesions. These research findings have been published in the latest issue of the Advanced Science journal.
The discovery of the KRAS gene in 1982 marked a significant breakthrough in cancer genetics. The research team's previous studies in 2019 and 2022 confirmed that a high-sugar diet is prone to causing sugar metabolism abnormalities in the pancreas, affecting nucleotide synthesis. This is a key factor in triggering DNA damage in pancreatic tissues/cells and leading to cancer-causing KRAS gene mutations (Research Reports: Protect Your Pancreas, Consume Less Sugar! / Sweet Trap: High-Sugar Diet Associated with Cancer Risk). However, the mechanisms by which KRAS mutations initiate the early formation of PanINs remained unclear. To unravel this mystery, the research team utilized 2-week-old KrasG12D/+ genetically modified mice and whole pancreas 3D tissue staining/scanning techniques for the first time, pinpointing the location of the earliest appearance of PanINs in the pancreas. (See Figure 1)
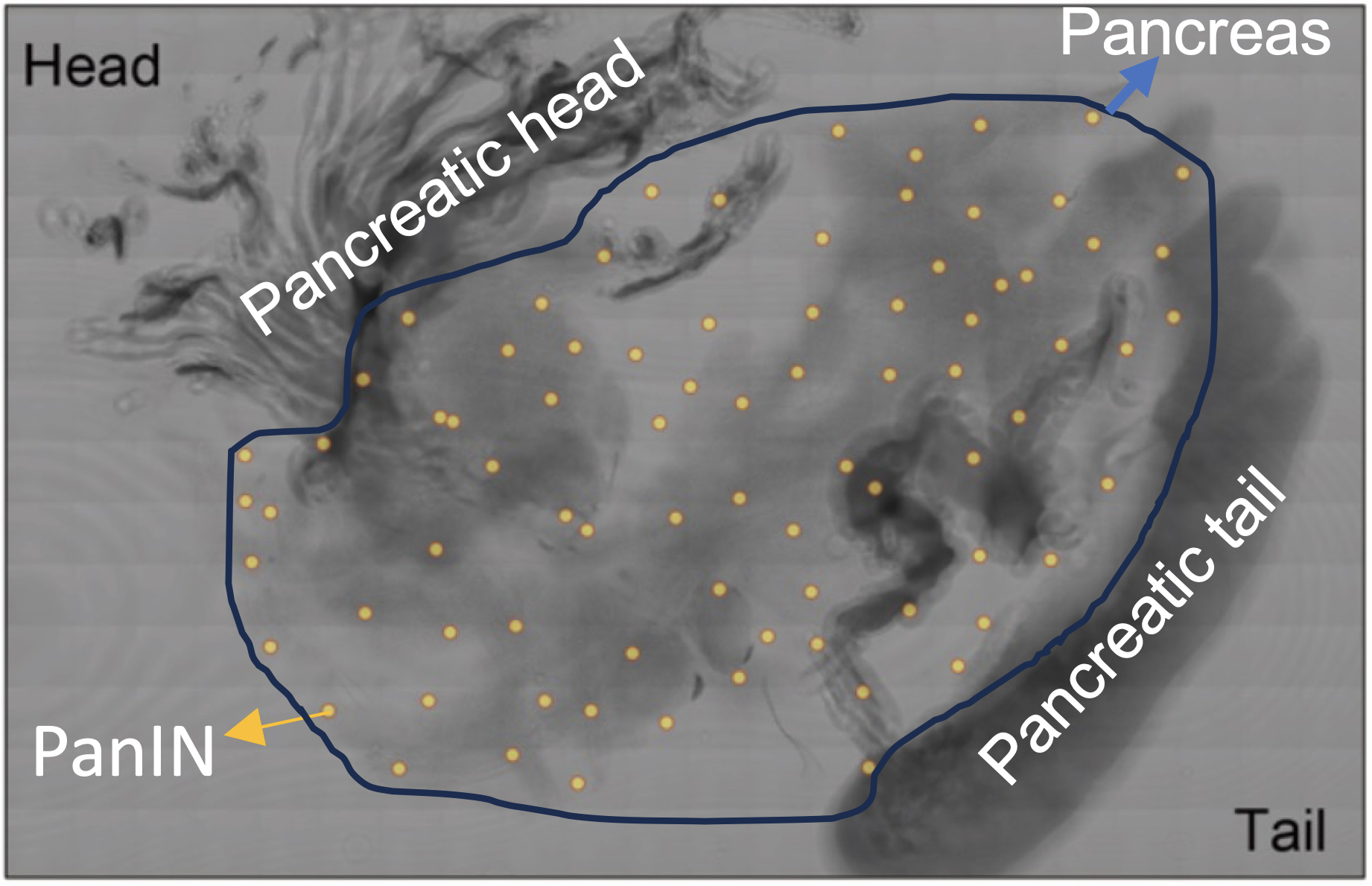 |
| Figure. Early-stage PanINs are randomly distributed in the pancreas of KrasG12D/+ genetically modified mice. |
The first author and corresponding author, Dr. Chun-Mei Hu, stated, "In the analysis of 50 KrasG12D/+ genetically modified mice, 5 mice showed no formation of PanIN, indicating our successful identification of the earliest occurrence of PanIN. Subsequently, by mapping the distribution of 45 formed PanINs on the same pancreatic tissue, we observed an interesting phenomenon: unlike the location of pancreatic cancer (which mainly occurs in the pancreatic head near the duodenum), early-stage PanINs are randomly distributed in the pancreas, suggesting that cellular genetic influences precede external environmental effects."
Researchers utilized microdissection techniques to isolate PanIN cells and surrounding normal pancreatic cells, conducting whole exome and RNA sequencing to analyze gene mutations and expression. They discovered that the Muc4 gene, a mucin, was the most significantly mutated and highly expressed gene, appearing in over 90% of KrasG12D/+ genetically modified mouse PanINs and human pancreatic samples with early-stage PanINs. Further isolating primary pancreatic cells from KrasG12D/+ genetically modified mice, they conducted experiments on Muc4 gene expression, confirming that the combined action of KrasG12D/+ and the Muc4 gene can initiate cellular transformation.
In examining the microenvironment around PanINs, it was observed that most PanINs were surrounded by activated fibroblasts. Culturing pancreatic cells expressing KrasG12D/+ and Muc4 genes directly with fibroblasts increased the carcinogenic characteristics of pancreatic cells, accelerating PanIN formation. Exploring the mechanism of their interaction further, it was found that KrasG12D/+ pancreatic cells, through genetic mutations, increased the expression of the Muc4 gene, thereby promoting cell proliferation.
Additionally, the collaborative overexpression of KrasG12D/+ and Muc4 genes stimulated pancreatic cells to release a small amount of growth hormone called Activin A, activating/recruiting fibroblasts, which then released a large amount of Activin A. This further enhanced the carcinogenic characteristics of pancreatic cells, initiating PanIN formation. (See Figure 2)
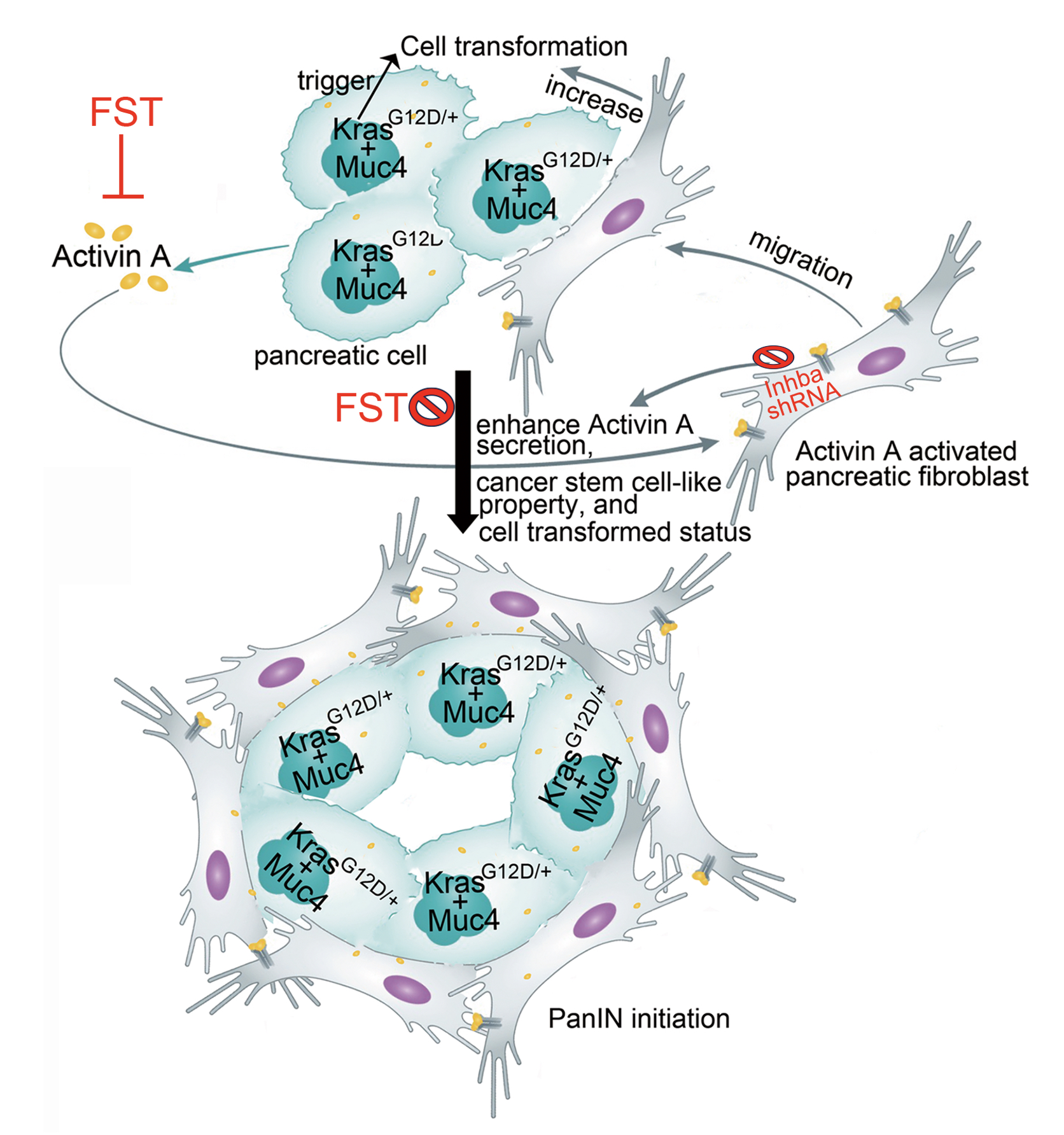 |
| Figure 2. When KrasG12D/+ and Muc4 genes collaborate, they promote cell growth and release a small amount of Activin A. This initiates and attracts fibroblasts, stimulating them to release more Activin A, further contributing to the carcinogenesis of pancreatic cells and the formation of PanINs (Pancreatic Intraepithelial Neoplasia). |
Previous studies have indicated that the absence of the Muc4 gene can prevent the formation of early pancreatic lesions (PanIN) and pancreatic cancer. Our research reveals that blocking the Activin A signal with follicle hormones can inhibit the activation and recruitment of fibroblasts in KrasG12D/+ genetically modified mice, thereby preventing the formation of PanIN. Additionally, reducing the expression of the Activin A gene in fibroblasts using gene knockout techniques also inhibits their ability to promote pancreatic cell carcinogenesis. This suggests that pancreatic cells overexpressing KrasG12D/+/Muc4 genes promote carcinogenesis by secreting Activin A, activating/recruiting fibroblasts, highlighting the crucial interaction between genetic mutations and induced microenvironmental changes in initiating early pancreatic lesions.
Looking back at 2022, the research team, in collaboration with medical institutions, analyzed clinical samples from pancreatic cancer patients. They found that when the expression of Activin A mRNA in fibroblasts surrounding cancer cells was higher, the malignancy and severity of the cancer in patients were more significant (research report: Cell-to-Cell Contact Key to Triggering Pancreatic Cancer Metastasis). In this study, clinical data from a database were incorporated, and it was observed that when both the MUC4 and Activin A genes were highly expressed in pancreatic cancer patients, their survival rates were lower than those with high expression of a single gene or low expression of both genes. Serum testing of pancreatic cancer patients revealed that higher levels of Activin A protein correlated with more malignant cancer grades and lower survival rates. Further analysis of the serum from high-risk groups with a family history of pancreatic cancer and early-stage pancreatic cancer patients showed higher levels of Activin A protein in cancer patients' serum. Moreover, as the severity of cancer increased, the content of Activin A protein in serum also increased (Figure 3). These research findings emphasize the significant roles of the MUC4 and Activin A genes in the initial formation of PanINs and the subsequent development of pancreatic cancer.
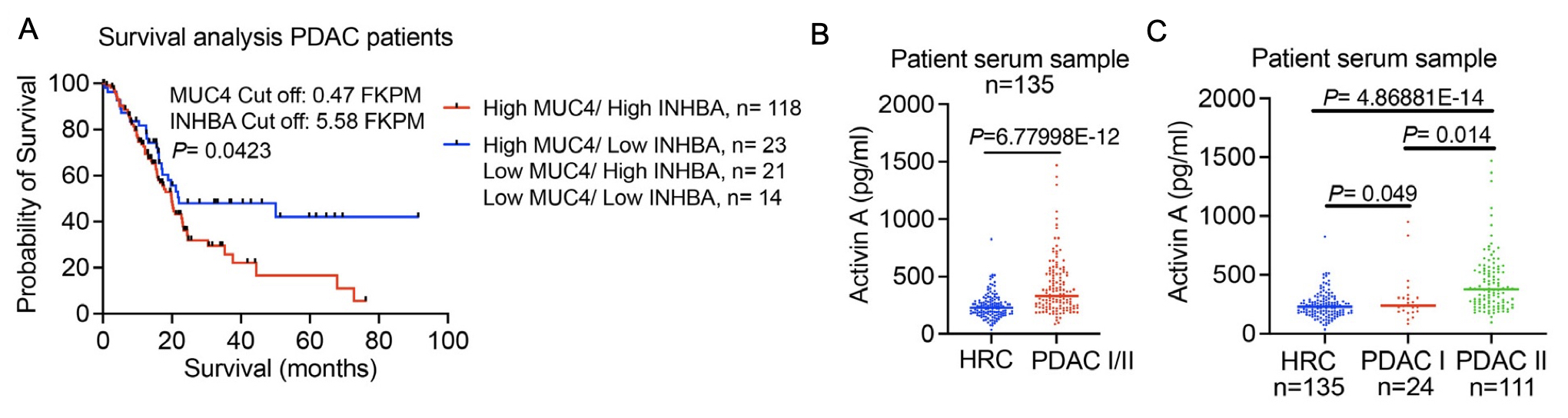 |
| Figure 3. (A) Relationship between the expression of MUC4 and Activin A genes (INHBA) and survival in pancreatic cancer patients. (B and C) Levels of Activin A protein in the serum of high-risk groups with a family history of pancreatic cancer (HRC) and patients with pancreatic cancer in stages I/II. |
Pancreatic cancer is challenging to detect in its early stages, progresses rapidly, and has poor prognosis. The findings of this study, for the first time, unveil the mechanism through which the oncogenic KRAS gene drives the initiation of pancreatic cancer precursors. The implications of this research can extend to detecting overexpression of the oncogenic MUC4 gene and secretion of Activin A. By blocking their signaling pathways using antibodies or small molecules, new strategies for early diagnosis and treatment of pancreatic cancer may be developed in the future.
This study was a collaborative effort, involving members such as Dr. Wen-Hwa Lee, Dr. Chun-Mei Hu, Dr. Chai-Ning Shen, Dr. Chien-Chang Huang, Dr. Hung-Jen Chien, and Dr. Yi-Ying Chen from the Genomic Research Center. Special thanks to Professor Shiue-Cheng Tang from National Tsing Hua University, and assistance provided by Dr. Yu-Ting Chang, Dr. Ming-Chu Chang, Dr. Yung-Ming Jeng, and Dr. Yu-Wen Tien from National Taiwan University Hospital.
A full study "Oncogenic KRAS, Mucin 4, and Activin A-mediated Fibroblast Activation Cooperate for PanIN Initiation" can be read online at: https://onlinelibrary.wiley.com/doi/epdf/10.1002/advs.202301240