Coronavirus-induced disease 19 (COVID‑19) infects more than three hundred and sixty million patients worldwide, and people with severe symptoms frequently die of acute respiratory distress syndrome (ARDS). In severe and fatal ARDS cases, SARS-CoV-2 infection has robust pulmonary inflammation and disproportionate immune response that may lead to high levels of circulating cytokines, intravascular coagulopathy, thrombotic tendency, and even multiple organ dysfunction.
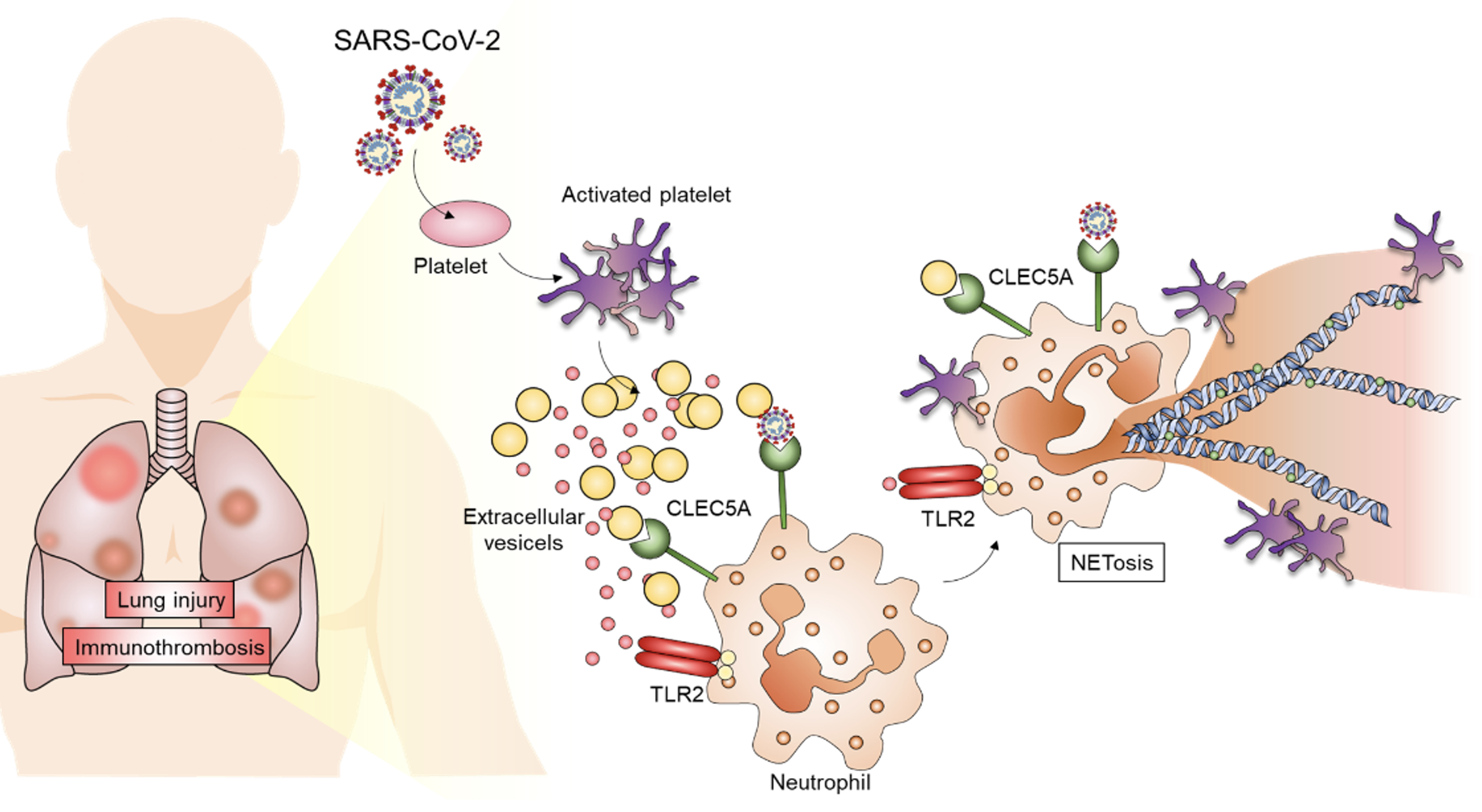
Thrombotic complication is a major cause of morbidity and mortality in patients with COVID-19, but the pathogenesis of thrombo-emboli formation is still unclear. In the current study, Dr. Edmond Hsieh and his team clearly demonstrate that PLT-EVs from COVID-19 patients can enhance thromboinflammation via CLEC5A and TLR2, two critical receptors in innate immunity, and further shows that PLT-EVs from virus-activated act as endogenous danger signals to cause systemic inflammation.
To this end, the research team pointed out CLEC5A and TLR2 are promising therapeutic targets to attenuate thromboinflammation and reduce the risk of post-acute COVID-19 syndrome in the future. This indepth article has recently been published in the journal of Biomedical Science.
“We found that platelets are hyperactivated in critically ill COVID-19 patients, and platelets-neutrophil interactions play critical roles in endothelial damage and immunothrombosis of COVID-19 patients,” explained research lead Dr. Hsieh.
SARS-CoV-2 infection is associated with increased platelet activation and platelet-neutrophil. Neutrophils are phagocytic immune cells contribute to early-phase viral clearance by forming neutrophil extracellular traps (NETs).
“We investigated SARS-CoV-2 infection is associated with higher neutrophil in infected tissues and high levels of proinflammatory cytokines leading to an extensive NETs formation with potential to propagate inflammation and microvascular thrombosis,” said Pei-Shan Sung, Ph.D., a postdoctoral researcher in the Dr. Hsieh’s Laboratory and first author of the study.
 |
| CLEC5A and TLR2 are responsible for SARS‑CoV‑2‑induced NET formation |
In previous work, Hsieh’s team has demonstrated that dengue virus (DV) and microbes bind and activate CLEC5A and TLR2 to release proinflammatory cytokines and promote NET formation. Because CLEC5A and TLR2 are associated and co-activated by platelet-derived EVs (PLT-EVs), It is becoming increasingly evident that CLEC5A and TLR2 also contributed to SARS-CoV-2-induced immunothrombosis.
To identify this approach, the researchers work on incubating SARS‑CoV‑2 with neutrophils in the presence or absence of platelets to observe NET formation. They isolated extracellular vesicles from COVID‑19 patients’ sera (COVID‑19‑EVs) and then incubated neutrophils with HC-EVs and COVID-19 EVs, respectively, to compare their abilities to induce NET formation.
Investigators found that while EVs from healthy control were unable to induce NET formation, COVID-19 EVs induced robust NET formation, which was blocked efficiently by anti-CLEC5A mAb. “This observation suggests that COVID-19 EVs have potent activity to induce NET formation via CLEC5A.” the team stated—the results could confirm the critical roles of CLEC5A and TLR2 in SARS‑CoV‑2‑induced lung inflammation in vivo.
In addition to thromboinflammation, SARS-CoV-2 infection resulted in lung injury and pulmonary fibrosis, including thicken of basement membranes and deposition of collagen. Thus, the team was interested to understand whether CLEC5A and TLR2 contributed to SARS-CoV-2-induced collagen deposition.
The researchers conducted their studies in mice that were genetically deficient CLEC5A and TLR2. At day 5 post-infection, severe thickening of alveolar cell wall and cell infiltration were noted in WT mice, while these phenomena were attenuated in mice deficient CLEC5A and TLR2 after SARS-CoV-2 infection.
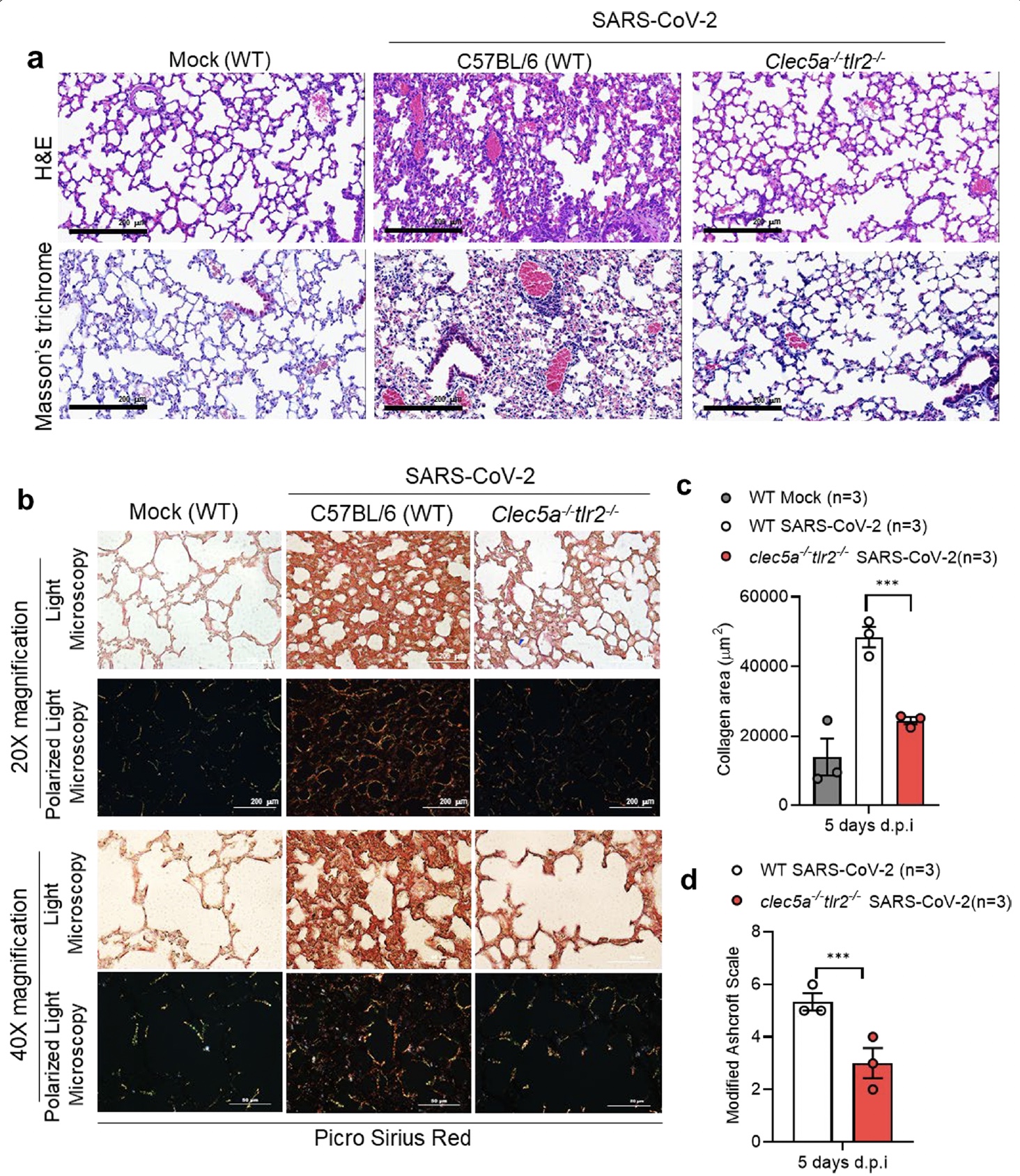 |
| CLEC5A and TLR2 are critical in SARS‑CoV‑2‑induced collagen deposition SARS‑CoV‑2‑challenged mice were sacrificed to harvest lung at 5 days post‑infection |
This study demonstrates that SARS‑CoV‑2‑activated platelets produce EVs to enhance thromboinflammation via CLEC5A and TLR2, and highlight the importance of CLEC5A and TLR2 as therapeutic targets to reduce the risk of ARDS in COVID‑19 patients. Dr. Edmond Hsieh speculates that their findings might be able to find a novel strategy to attenuate virus-induced lung inflammatory reactions in the future.
The paper titled “CLEC5A and TLR2 are critical in SARS-CoV-2 induced NET formation and lung inflammation” can be read online at: https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-022-00832-z