Background: Coronavirus-induced disease 19 (COVID-19) infects more than three hundred and sixty million patients
worldwide, and people with severe symptoms frequently die of acute respiratory distress syndrome (ARDS). Recent
studies indicated that excessive neutrophil extracellular traps (NETs) contributed to immunothrombosis, thereby
leading to extensive intravascular coagulopathy and multiple organ dysfunction. Thus, understanding the mechanism
of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-induced NET formation would be helpful to reduce
thrombosis and prevent ARDS in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
Methods: We incubated SARS-CoV-2 with neutrophils in the presence or absence of platelets to observe NET formation.
We further isolated extracellular vesicles from COVID-19 patients’ sera (COVID-19-EVs) to examine their ability to
induce NET formation.
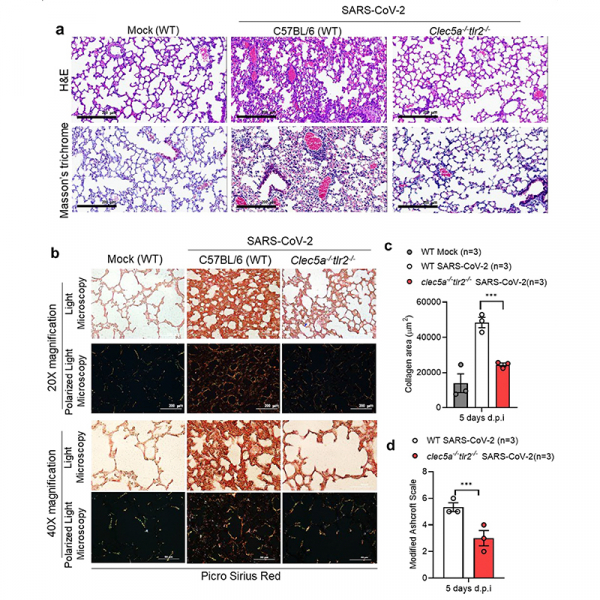
Results: We demonstrated that antagonistic mAbs against anti-CLEC5A mAb and anti-TLR2 mAb can inhibit COVID-
19-EVs-induced NET formation, and generated clec5a−/−/tlr2−/− mice to confirm the critical roles of CLEC5A and TLR2
in SARS-CoV-2-induced lung inflammation in vivo. We found that virus-free extracellular COVID-19 EVs induced robust
NET formation via Syk-coupled C-type lectin member 5A (CLEC5A) and TLR2. Blockade of CLEC5A inhibited COVID-19
EVs-induced NETosis, and simultaneous blockade of CLEC5A and TLR2 further suppressed SARS-CoV-2-induced NETosis
in vitro. Moreover, thromboinflammation was attenuated dramatically in clec5a−/−/tlr2−/− mice.
Conclusions: This study demonstrates that SARS-CoV-2-activated platelets produce EVs to enhance thromboinflammation
via CLEC5A and TLR2, and highlight the importance of CLEC5A and TLR2 as therapeutic targets to reduce the
risk of ARDS in COVID-19 patients.